- [email protected]
- 27-31 Wright St, Clayton VIC 3168
- Contact
01Oct
World’s first eye transplant was a giant leap forward—but vision remains elusive
by Elazadeh, 0 Comments
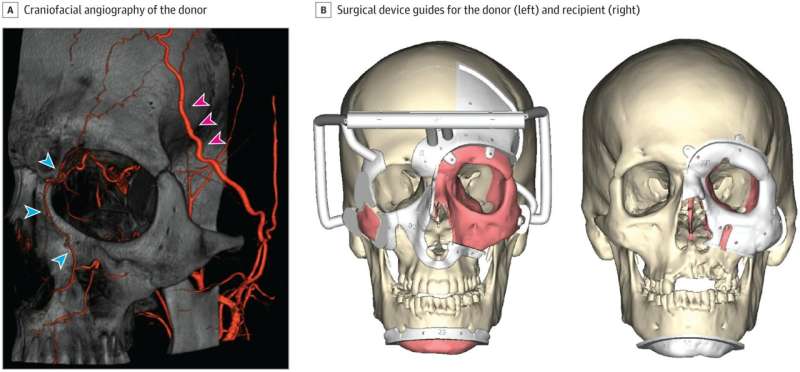
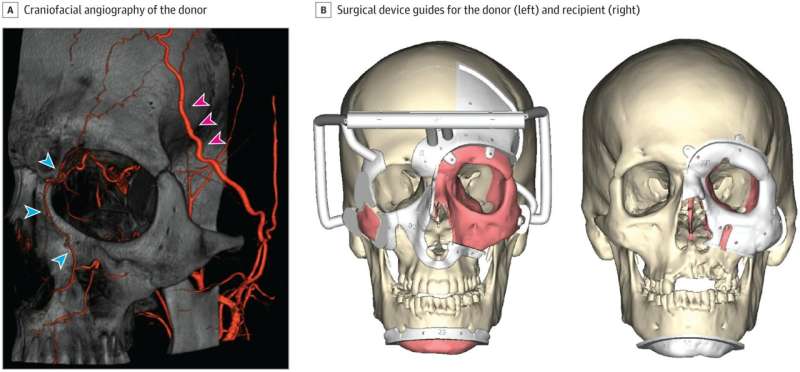
Perioperative Planning and Intraoperative Details of the Combined Whole Eye and Face Transplant Procedure. Credit: JAMA (2024). DOI: 10.1001/jama.2024.12601
Three years ago, Aaron James, a utility lineman, lost half of his face and his arm when he was struck by a high-voltage electrical cable.
Last year, the 47-year-old received a face and whole-eye transplant—the first of its kind. The surgery took 21 hours and involved 140 health care professionals.
James is making remarkable progress, as recently reported in JAMA, a medical journal. Although he cannot see out of the transplanted eye, it continues to maintain normal pressure and blood flow—and it hasn’t shrunk (something that happened when eye transplants were previously attempted in animals). Doctors said the surgery laid the “foundation for further advancements and ongoing research.”
While face transplants have been done previously, they have only a relatively recent entry into surgical history with the first partial transplant occurring in 2005 and the first full transplant in 2010. As of September 2023, 50 of these surgeries have been undertaken, globally.
Tens of thousands of corneal transplants—partial eye transplants—are done every year. But this is a much more straightforward operation.
Why can’t eyes be easily transplanted?
For a start, eyes are held in place by many strap-like muscles that help to move the eye around, and myriad small blood vessels keep the muscles and tissues of the eye alive. There is also a second far more complex reason eyes are difficult to transplant: the optic nerve.
The optic nerve carries electrical information to the visual cortex of the brain. This nerve is an extension of the central nervous system, so taking one eye and its associated nerve and trying to connect it to another brain is not straightforward.
To put it in numbers, it would probably be the most difficult rewiring job anyone had ever undertaken because about 1.2 million nerve cells contribute to the optic nerve. Matching up each of these to the relevant optic nerve and visual cortex of the brain of another person is almost impossible, especially because there are probably differences in the exact number of nerves contributing to the nerve from person to person. Each nerve is responsible for a small area of what you see, mapping to a specific area in the brain.
This incoming light energy triggers a biochemical cascade to convert it into electrical energy by the photoreceptor cells in the retina. The electrical energy is transported to the back of the brain and built into an image that we see.
To add to this complexity, some light information from each eye ends up on the opposite side of the brain to help build a complete picture. And information is cast into your eye upside down, so the brain fixes that too by working with the vestibular system (a system in the inner ear that provides balance and sense of orientation) so that we interpret everything the right way up.
The retinal cells inside the eye are also another complicating factor. They are incredibly delicate and require a constant blood supply. Without the oxygen it brings, they die in as little as 12 minutes. To solve this issue, the surgeons who operated on James ensured the blood supply to the donated eye was maintained.
[embedded content]
What about nerve repair or regrowth?
There are considered to be two nervous systems in our body: the central nervous system, which encompasses the brain, spinal cord including the retina of the eye, and the peripheral nervous system, which is pretty much everything else.
It is well known that nerves in the central nervous system have a very limited ability to repair. There is lots of evidence of this from millions of people who have had traumatic eye injuries, where the retina has been damaged and resulted in vision loss.
Might we eventually be able to restore vision?
It’s difficult to say. However, there are interesting studies in animals that suggest that reactivating embryonic signaling pathways, is the process that drives stem cells in our body as we develop to become different cells of the body (in this case, retinal cells) might help repair nerves. Other vertebrates, such as newts and zebrafish, are able to repair their retina, even following significant damage.
Stem cells have shown amazing results in repairing blindness caused by damage to the outside layer (the cornea) of the eye, particularly where a person has damaged one eye. Stem cells from the healthy eye can be removed, grown in a lab and then transferred to the injured eye to repopulate and repair the damaged cornea, restoring functionality.
Where both eyes are injured, donor stem cells from the eye of a fresh cadaver may be used. But the recipient needs to take immunosuppressant drugs for the rest of their life. This can cause complications, such as increasing the risk of viral, bacterial or fungal infections.
As for James, the retinal cells of his transplanted eye respond to light and information is being processed along the visual pathway. Unfortunately, this doesn’t translate to vision—but then, that was never the expectation.
So when it comes to whole-eye transplantation, progress is being made, but there are still significant difficulties to overcome. This procedure, however, is another milestone in the remarkable journey of one man and another milestone in the surgical achievements of transplantation.
Journal information:
Journal of the American Medical Association